Medicaid Work Requirements – Update
Momentum is growing in Congress on requiring state Medicaid programs to implement work or community engagement requirements (with some exemptions) for certain Medicaid recipients, specifically working-age adults who are considered able-bodied.
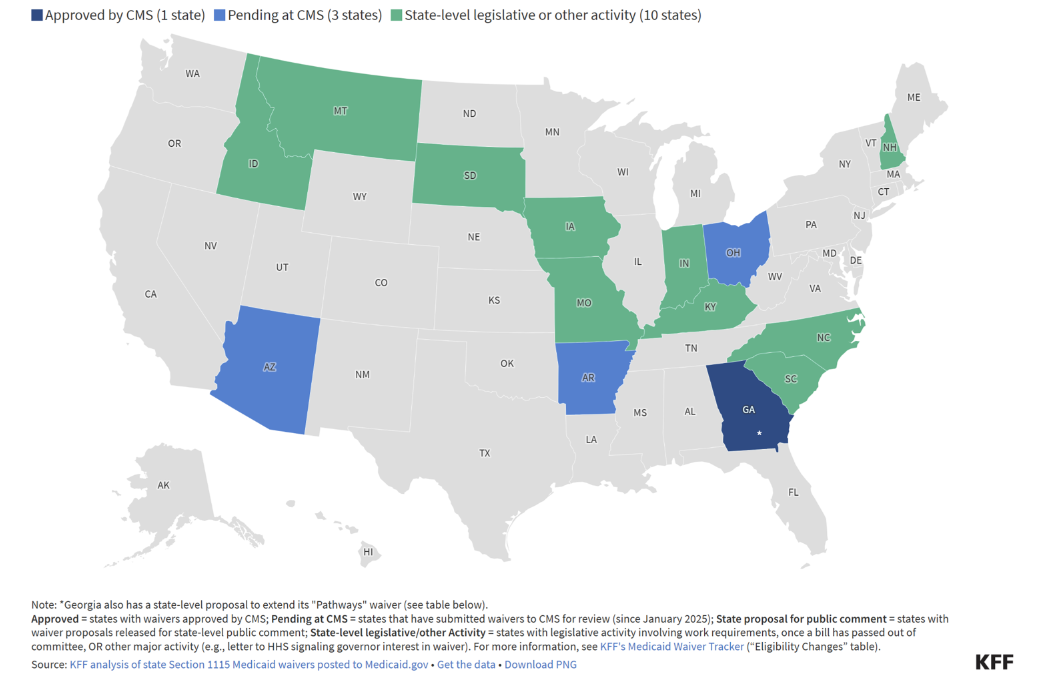
In advance of a new mandate for Medicaid work requirements, 14 states are already actively pursuing a work/community engagement requirement for their programs. (See below map). Three of these states have already submitted Section 1115 waiver applications to the Centers for Medicare and Medicaid Services (CMS), while 10 others are preparing for a work requirement by enacting enabling legislation or revising administrative rules. Georgia stands out as the only state with an active work requirement program targeting adults (up to 100 percent of FPL) who otherwise would not be eligible for Medicaid, as Georgia has not expanded Medicaid under the Affordable Care Act (ACA).
At the federal level, discussions around Medicaid work requirements have been a focal point in the House of Representatives as part of broader efforts to achieve over $700 billion in cost savings in the Medicaid federal budget over 10 years. [1] On May 22, 2025, the House passed a comprehensive budget bill that, if passed by the Senate, would require states to implement rules mandating “community engagement” by able-bodied childless adults aged 19–64 by December 31, 2026.[2],[3]
Under these new community engagement rules, individuals would have to demonstrate completion of 80 hours per month of work, community service, educational programs and/or work programs in the month prior to applying for Medicaid benefits. The bill includes provisions to exempt certain groups from these requirements, such as individuals who are pregnant, eligible for postpartum coverage, or recently released from incarceration. The House bill also allows states to add short-term hardship exemptions, such as for hospitalization or natural disaster. In addition to community engagement requirements, the bill would require states to redetermine these individuals’ eligibility for Medicaid every six months, an increase in frequency from the current annual requirement.
Recognizing the potential challenges states may encounter in implementing the community engagement provisions, the House bill allocates $100 million in grants to the states to support the preliminary work for implementing the community engagement requirements. This funding would be allocated in federal fiscal year 2026 in proportion to each state's share of Medicaid enrollees subject to the new community engagement requirements.
A recent analysis conducted by the Urban Institute for the Robert Wood Johnson Foundation[4] estimates that federal work requirements could impact approximately 5 million adults — out of the more than 13 million who have Medicaid coverage in the 40 states (plus Washington, D.C.) that expanded their Medicaid coverage under the ACA. These individuals could face the risk of losing their benefits if they are unable to meet the new requirements, show documentation of compliance, or document their qualification for an exemption.
As previously outlined in A&M’s analysis on Medicaid work requirements,[5] states must employ strategies to design and implement these policies in a way that balances the goals of encouraging workforce participation or community engagement while maintaining access to essential health coverage for vulnerable populations. Key planning and implementation considerations include:
- Concretely defining the state's goals and objectives for implementing work requirements
- Describing who is subject to work requirements, what criteria will be used to identify these individuals (e.g., age, income, or eligibility category), and how their compliance will be verified
- Establishing who will perform functions needed for identifying included and excluded individuals, documenting their compliance or exception, and deciding whether vendor support is needed
- Confirming how states will use technology to automate identification and verification processes, which are heavily dependent on availability of data and data system structures
- Defining consequences for not meeting the requirements and what the appeals process for losing benefits or exclusion status will look like
While the implementation of Medicaid work requirements represents a significant shift in policy, states can manage this change with careful planning and execution to ensure that vulnerable populations retain access to essential health coverage.
How A&M Can Help
A&M’s team of Medicaid experts can provide critical support to states as they work to integrate work requirements successfully into their existing Medicaid programs. By leveraging expert guidance and adopting a strategic framework, states can address these challenges and create sustainable Medicaid programs that align with both federal mandates and the needs of their populations.
[1] Alis Hingham, “Donald Trump's Spending Bill Makes Progress as Medicaid Faces Cuts,” Newsweek, May 19, 2025, https://www.newsweek.com/donald-trump-spending-bill-progress-medicaid-cuts-2073954
[2] House Resolution 1 – One Big Beautiful Bill Act, Section 44141, https://www.congress.gov/bill/119th-congress/house-bill/1/text
[3] Emily Brooks, “GOP leaders reveal changes to win over holdouts on Trump agenda bill,” The Hill, May 22, 2025, https://thehill.com/homenews/house/5313019-salt-medicaid-house-republicans-trump-bill/
[4] M. Karpman et al., “How Work Requirements Would Affect Medicaid Coverage in Each Expansion State,” Robert Wood Johnson Foundation, April 14, 2025, https://www.rwjf.org/en/insights/our-research/2025/04/how-work-requirements-would-affect-medicaid-coverage-in-each-expansion-state.html
[5] “Getting Medicaid Work Requirements Right,” Alvarez & Marsal, accessed May 27, 2025, https://www.alvarezandmarsal.com/sites/default/files/2025-01/45487_PS_Medicaid%20Work%20Requirements%20TL.pdf







