Preparing for Potential Disruptions in Federal Funding
The Trump Administration's Executive Order to reduce NIH indirect funding to 15% for institutions conducting medical research including hospitals and universities, has generated significant uncertainty among healthcare providers. Academic Medical Centers (AMCs) and Schools of Medicine rely heavily on NIH grants not just for research projects, but also for the operational costs that support their research infrastructure. With the cap at 15%, many health systems and AMCs will face financial strain which could impact their ability to deliver on their mission, including stifling scientific advancement, and diminishing the quality of medical education and patient care available.
Healthcare organizations should take action now to best prepare their organizations for the future.
Action 1: Assess Space and Resource Efficiency
- Maximize Space: Comprehensively assess facility’s footprint, breaking it down by wet lab, dry lab, and administrative spaces. Identify underutilized areas, to develop actionable strategies to increase efficiency and monetize excess capacity, turning overlooked assets into revenue-generating opportunities.
- Enhancing Administrative Efficiency: Streamline administrative functions across departments by developing new shared services opportunities.
- Streamline and Consolidate: Consolidate redundant services to drive cost savings and improve operational performance including technology and core labs.
Action 2: Optimize Your Workforce
- Strategic Workforce Optimization: Perform a detailed workforce analysis to identify opportunities to reduce unnecessary overhead expenses, including strategic right-sizing (RIF) initiatives to align staffing with institutional needs while maintaining high-quality care and research output
- Optimize Faculty Deployment (CARTs): Analyze current faculty deployment to identify gaps in funded research efforts. Evaluate opportunities to reduce unfunded research burdens, by developing solutions that enhance faculty productivity while improving financial efficiency and access.
- Strategic Recruitment Planning: Develop a five year horizon faculty deployment plan reflective of current landscape
Action 3: Drive Margin Transformation
- Expense Classification and Financial Optimization: Align cost structures with best practices by classifying expenses correctly and identifying misallocations to optimize financial reporting.
- Driving Margin Improvement for Health Systems: Through targeted transformation efforts, implement strategies to reduce operational costs and improve margins.
Action 4: Optimize Your Research Portfolio
- Conduct an in-depth assessment of your research portfolio: Identify areas for rationalization or strategic shifts in funding priorities. Align your research investments with institutional strengths and market opportunities, ensuring sustainable growth.
Action 5: Revitalize Donor Engagement
- Private funding is a critical component of long-term success: While fundraising efforts often reside within the university, evaluate strategies to improve donor engagement, align philanthropic initiatives with institutional priorities for maximum impact.
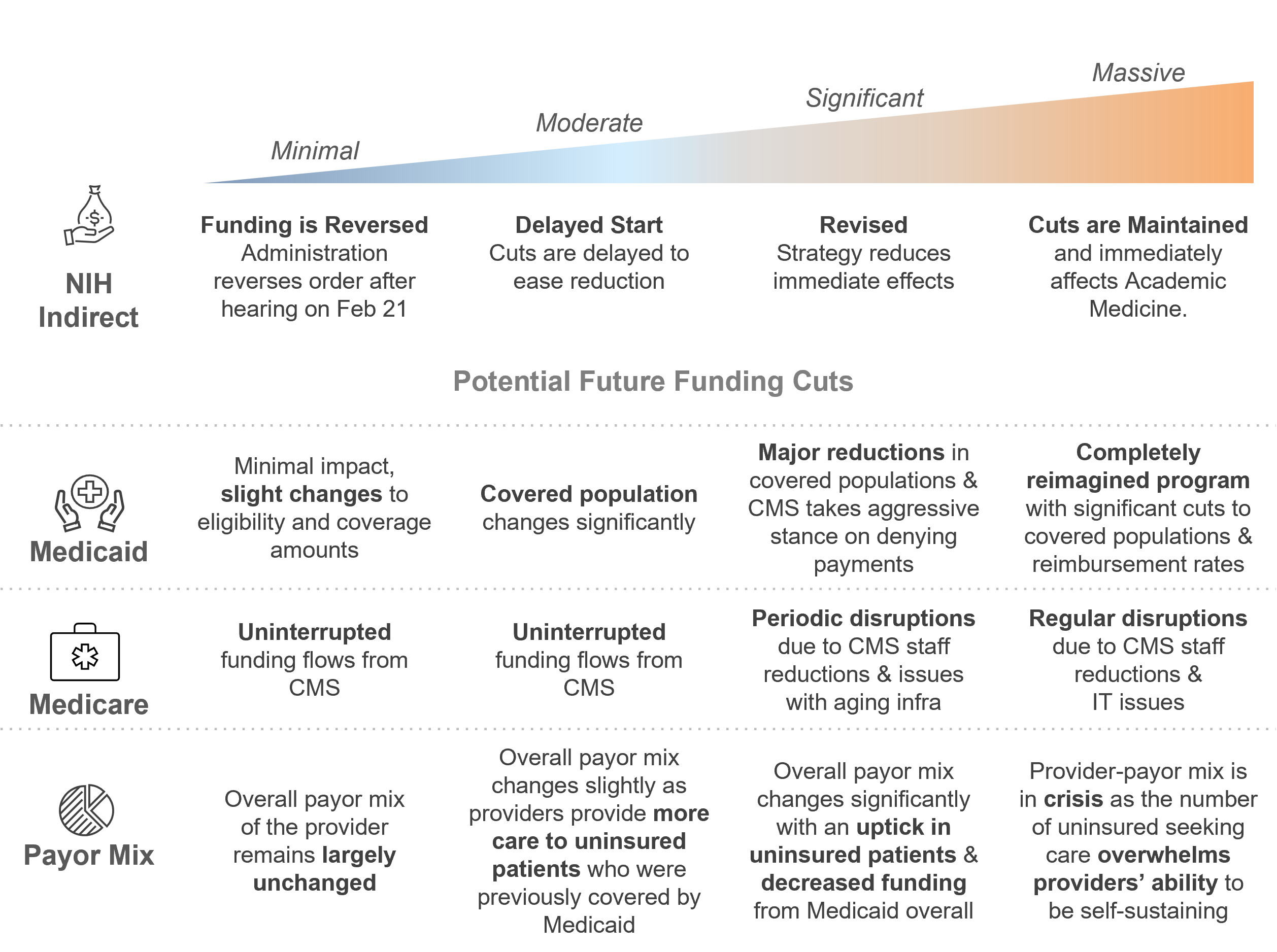
The Healthcare Disruption Continuum
The volatility of the healthcare industry will continue to increase over the next six months with the actions and anticipated measures of the Trump Administration, Department of Government Efficiency (DOGE), and proposals currently being considered by various Congressional Committees. This volatility can be charted out across a Disruption Continuum (pictured below) that health care providers can use to evaluate forthcoming changes and implement strategies to maintain capacity to deliver care in a financially sustainable way.
With universities reporting hundreds of millions in loss of funding, our professionals have the ability to assist in developing custom, tailored strategies to maximize operational efficiency, optimize resources and drive financial sustainability. It is imperative that providers act now to proactively prepare for these imminent disruptions.



