Utilization and Case Management Programs: Linchpins to Provider Success in an At-Risk Reimbursement Environment
Centers for Medicaid and Medicare Services (CMS) has taken a leading role in reforming Medicare, and by default, the entire healthcare system; i.e., Medicare is often seen as the bellwether for reimbursement change by commercial payers. Last year, on January 26, 2015, Secretary Sylvia Burwell of Health and Human Services (HHS) established a timeline for moving from volume to value: “Our first goal is for 30 percent of all Medicare provider payments to be in alternative payment models that are tied to how well providers care for their patients, instead of how much care they provide — and to do it by 2016. Our goal would then be to get to 50 percent by 2018. Our second goal is for virtually all Medicare fee-for-service payments to be tied to quality and value; at least 85 percent in 2016 and 90 percent in 2018.”1
Emerging business models necessitate a care delivery model focused on the total cost of care, while ensuring outcomes inclusive of clinical performance, the experience of care and ready access. The advent of a value-oriented payment system (e.g., Accountable Care Organizations, Comprehensive Care Joint Replacement model) requires that the “right” patient receives the “right” care in the “right” place at the “right” time by the “right” provider.
The accelerating use of outcome-based payments, Medicare and other payers mandates a “hands on” evidence-based and integrated approach to care delivery. In this article, we discuss the growing role of case and utilization management, supported by analytics, in the value creation process.
Aging population driving CMS payment reform and restructuring of care delivery
From 2015 to 2025, the number of individuals over the age of 65 is forecast to increase from 47.7 million (14.8 percent of the total population) to 65.1 million (18.8 percent).2 The aged account for disproportionate healthcare spending, with Medicare expenditures per fee-for-service (FFS) aged beneficiary increasing with each age cohort (65–74: $7,859; 75–84: $12,805; over 85: $13,788).3 Higher spending is consistent with an increase in the number and severity of co-morbid chronic conditions and the high cost of end-of-life care. Medicare FFS spending is also highly concentrated, with 10 percent of beneficiaries accounting for 57 percent of spending; the least costly 50 percent of beneficiaries account for 5 percent of spending.4 Per capita (beneficiary) inpatient hospital spending of $3,695 accounts for 46.4 percent of total spending.5
Utilization management: From oversight to discharge planning and provider variation
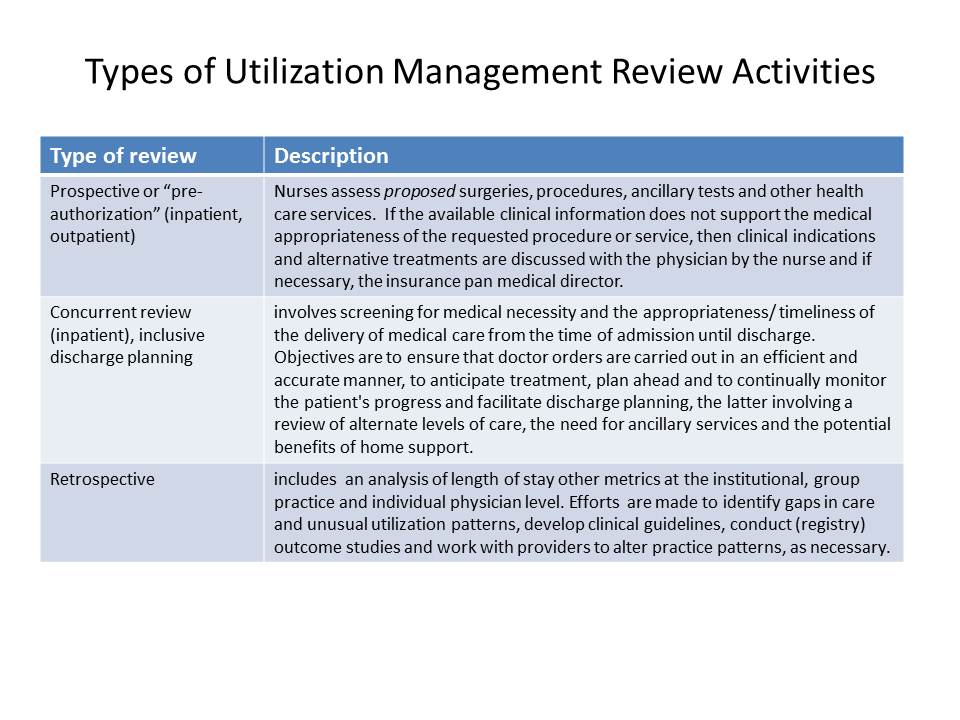
Utilization management (UM) represents an evidence-based, clinical support process to assist physicians, other providers and payers in evaluating the use of medical services based on medical necessity, appropriateness and efficiency.6 UM may be performed prospectively, concurrently and retrospectively. Historically, UM has been viewed as a means to reduce costs in a volume-driven, fee for service outpatient and DRG-driven inpatient healthcare market. The emerging, at-risk care delivery system presents an opportunity for an effective UM program to benefit providers and patients through enhanced discharge planning, reduced provider variation and continually improved process-of-care.
The advent of Accountable Care Organizations, value-based purchasing readmission penalties and episode-based reimbursement highlight the importance of patient discharge destination. In 2012, there were 13.7 million hospital discharges of people over age 65: 48.0 percent were sent home, 43.6 percent received post-acute care services (i.e., skilled nursing facility, home health care, inpatient rehab facility, long-term acute care hospital), 3.2 percent died and 2.2 percent transferred to another hospital.7 A risk-adjusted analysis of destination sites highlights a broad range of spending without a commensurate relationship to health outcomes.
Significant variation exists in the utilization of acute inpatient, post-acute and outpatient services by physician exists. Inpatient variation is notable for specific risk-adjusted conditions in terms of length of stay, complications, mortality, use of ancillary resources (e.g., imaging, labs), outpatient / observation stays, admission rates, gaps in care and other conditions. Post-acute variation is notable for its site of service, length of stay, complication and re-admission rate. Variation in the ambulatory care sensitive hospitalization rate suggests opportunities for improved chronic disease management. Physician-led peer review (utilization management) and teamwork for high-value care is an essential component of the Mayo Clinic’s group medical model.8
Case management: Optimizing health management and outcome, while lowering costs
Case management targets high cost and moderate-to-high-risk patients consuming a disproportionate amount of health care resources. In the Medicare fee-for-service (FFS) population, 1 percent of patients accounts for 15 percent of spending, the next 4 percent accounts for 24 percent for a total of 5 percent of patients accounting for 39 percent of expenditures.4 Effective case management programs are becoming increasingly important in a healthcare system being impacted by a variety of factors including an aging population, re-admission penalties, increased quality reporting requirements, ACO enrollment growth, expanded health insurance coverage, payment reform and importantly, a growing shortage of primary care physicians.9
Case managers have a difficult and multifactorial role focused on prevention, proactive intervention and transitions of care. They facilitate care for complex patients with complex chronic co-morbid conditions and/or psychosocial needs, coordinate care to assure quality outcomes in the most cost-effective manner, reduce avoidable hospital admissions, reduce gaps in care, impact practice quality scores and engender self-management capabilities; i.e., the ability to identify changes in health status and be compliant with a treatment plan. They require timely access to data, information and insights regarding patient status.
The misalignment of financial incentive poses challenges to case managers employed by health systems and hospitals. Site of service reimbursement differentials have increased between offerings provided by hospital outpatient clinics (e.g., diagnostic imaging, echocardiograms, ambulatory surgical centers, oncology drug infusion centers) and non-hospital private practice providers. Lower cost care (of equal quality) that would potentially reduce the revenues of the case manager’s employer is often available in the community. The misalignment issue still requires resolution.
Opportunities also exist for case managers to become increasingly engaged with palliative and hospice care, as 25–30 percent of Medicare expenditures are spent in the last year of life; the average cost in the final year of life, $82,343 as calculated by A&M, is 10 times the cost of surviving Medicare recipients.10,11 Our calculation is based on a previously published estimate of last year of life costs as a percentage of total Medicare spending and the number of deaths in the population over age 65 irrespective of cause.11
Case & utilization management without timely, actionable and data-driven insights of limited value
Healthcare providers, especially hospitals, have made substantial investments in electronic medical record systems, inclusive of clinical, administrative, financial and operational functionality. However, challenges remain regarding interoperability with legacy and other IT systems, implementation to hospital-employed and affiliated physicians, data extraction and physician acceptance. Electronic medical records (EMRs) were touted as tools to enhance physician productivity, and yet their design appears more oriented toward administrative processes, ancillary staff, redundancies and billing.
Effective case and utilization management across the continuum of care requires timely, actionable and data-driven insights to ensure pro-active intervention. The insights may potentially be derived from hospital, ambulatory care, laboratory and pharmaceutical data via health exchanges that are accessible to critical members of the care team on a real-time basis.
Behavioral connectivity: An emerging unmet need for case management
Consumer behaviors and social circumstances account for 55 percent of the determinants of premature death, the remainder being genetic predisposition, and environmental factors and health.12 The Institute of Medicine has defined self-management as the “systematic provision of education and supportive interventions by health care staff to increase patients' skills and confidence in managing their health problems, including regular assessment of progress and problems, goal setting, and problem-solving support.“ This may include the self-monitoring of symptoms, responding with appropriate actions when symptom levels indicate a problem, adhering to medication regimens, making major lifestyle changes, and scheduling visits for lab tests, physical exams and clinical consultations, as needed.
Case managers are well-positioned within the healthcare system to facilitate patient and caregiver engagement; improved health outcomes and lower costs are likely.
Registered nurses critical to case and utilization management
In 2012, there were approximately 2.9 million registered nurses (Diploma: 16 percent, Associates: 37 percent, Bachelors or higher: 47 percent), of which 85 percent are working in nursing.13,14 The majority of working nurses are employed by hospitals (62 percent), followed by ambulatory care (11 percent), public / community health organizations, including schools and clinics (8 percent), home health (6 percent) and nursing homes (5 percent).14 The percentage of working nurses over the age of 50 years is 53 percent, with a high rate of attrition (nearly 77,000 per year driven largely by retirements).15,16 The attrition of older, experience nurses is being offset by the rise in nursing school graduates per year from 68,759 in 2001 to 155, 098 in 2013.13
The magnitude of nursing shortages at the national level remains unclear. Recent forecasts vary widely, with a projected shortage of 918,232 nurses by 2030 (Digital Commons) to a surplus of 340,000 by 2025 (Bureau of Health Workforce).13,17 However, all agree that regional variation in supply-demand is significant and that many states will have nurse shortages, particularly in states with rapid (percentage) growth in the over 75 age cohorts, where the demand for health services increases at the greatest rate. Among the cited states, mostly in the west, with the largest shortages are Arizona, Colorado, Maryland, Nevada, New Mexico, Oregon and Rhode Island.
Recruiting experienced case and utilization managers may be increasingly challenging given the attrition rate and shortages in selected states.13 Higher than average salaries may be required, but appear justifiable given the potential for cost savings. Inadequate case and utilization management focus and staffing may lead to higher costs and/or lower quality.
Summary
Payment reform from volume to value will substantially increase the relative importance to providers of population health initiatives to identify and stratify high cost / risk patients for discharge planning and case management, as well as the need for a reduction in episode variation (e.g., joint replacement) in the total cost of care. A disciplined and organized care management process focused on generating quality outcomes across the continuum is essential.
Fully-staffed utilization and case management programs are the linchpin to the emergence of a seamless, fully integrated care delivery model that is better able to: match patient acuity with the appropriate level of post-acute and outpatient care; manage transitions among alternative sites of care; facilitate evidence-based approaches to minimize gaps in care; and promote patient (caregiver) self-management.
Essential elements of utilization and case management include human capital strategies (i.e., leadership, recruitment, organizational development and staff performance optimization); proactive collaboration among patients, payers, primary care physicians and clinical specialists; supportive cloud-based technology applications; data analytics; and regulatory compliance.
About A&M’s Clinical Support Services (CSS) Practice
A&M’s CSS practice provides experienced RNs for leadership and staff positions in utilization and case management. Personnel are immediately available to organizations with short-term operational and longer-term, strategic needs. Our CSS team is able to support the operational needs of providers and payers across the entire care continuum.
1HHS Press Office. Better, Smarter, Healthier: In historic announcement, HHS sets clear goals and timeline for shifting Medicare reimbursements from volume to value; January 26, 2015
2U.S. Census Bureau.
3Medicare Data Book, June 2015, Chart 2-2: Medicare enrollment and spending by age group, 2011 http://medpac.gov/documents/data-book/june-2015-databook-health-care-spending-and-the-medicare-program.pdf?sfvrsn=0
4Medicare Data Book, June 2015, Chart 1-10: FFS program spending is highly concentrated in a small group of beneficiaries, 2011 http://medpac.gov/documents/data-book/june-2015-databook-health-care-spending-and-the-medicare-program.pdf?sfvrsn=0
5Medicare Data Book, June 2015, Chart 1-2: Per capita Medicare spending among FFS beneficiaries, by sector, 2004–2013, http://medpac.gov/documents/data-book/june-2015-databook-health-care-spending-and-the-medicare-program.pdf?sfvrsn=0
6Flemmons K, Wyatt P. Utilization Management: CMS Guidelines for Observation and Inpatient Services. Presentation from Vanderbilt University Medical Center; February 2, 2015.
7Medicare Data Book, June 2014, Chart 6-15. Discharge destination of Medicare fee-for-service beneficiaries, 2006–2012 http://medpac.gov/documents/publications/jun14databookentirereport.pdf
8Mayo Clinic: Multidisciplinary Teamwork, Physician-Led Governance, and Patient-Centered Culture Drive World-Class Health. The Commonwealth Fund Case StudyOrganized Health Care Delivery System; August 2009 http://www.commonwealthfund.org/~/media/Files/Publications/Case%20Study/...
9Auslander E, Cameal G. 10 Healthcare reform issues transforming case management.
10Calfo S., Smith J., Zezza. CMS Office of the Actuary: Last Year of Life Study, 2001. Note, 2001 estimates applied by A&M to 2013 Medicare expenditures as determined by CMS
11CMS National Health Expenditures https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/index.html; and Deaths: Leading Causes for 2012. National Vital Statistics Reports, Volume 64 (10); August 31, 2015 http://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_10.pdf
12Schroeder. We Can Do Better. NEJM 2007; 357: 1221-1228
13HHS, Bureau of Health Workforce, National Center for Health Workforce Analysis. The Future of the Nursing Workforce: National- and State-Level Projections, 2012-2025 http://bhpr.hrsa.gov/healthworkforce/supplydemand/nursing/workforceprojections/nursingprojections.pdf
14The Registered Nurse Population: Findings from the 2008 National Sample Survey of Registered Nurses; September 2010 http://bhpr.hrsa.gov/healthworkforce/rnsurveys/rnsurveyfinal.pdf
15American Nurses Association. FAST FACTS. The Nursing Workforce 2014: Growth, Salaries, Education, Demographics & Trends http://www.nursingworld.org/MainMenuCategories/ThePracticeofProfessionalNursing/workforce/Fast-Facts-2014-Nursing-Workforce.pdf
16Spetz J. Too Many, Too Few, or Just Right? Making Sense of Conflicting RN Supply and Demand Forecasts. NURSING ECONOMIC$, Volume 33(3); /May-June 2015 177
17Digital Commons. United States Registered Nurse Workforce Report Card and Shortage Forecast, January 2012 http://digitalcommons.unl.edu/cgi/viewcontent.cgi?article=1148&context=publichealthresources