Behavioral Health and the Total Cost of Care
“The good physician treats the disease; the great physician treats the patient who has the disease.”1 Sir William Osler
According to the definition suggested by the Patient-Centered Primary Care Collaborative, “behavioral health is an umbrella term for care that addresses any behavioral problems impacting health, including mental health and substance abuse conditions, stress linked physical symptoms, patient activation and health behaviors.”2
The advent of payment reform, implementation of the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA), an alarming increase in the number of drug-related overdose deaths, and growing recognition of the financial impact of behavioral health on the total cost of care have refocused payers, providers and patients on the need for integrated behavioral-medical care.
In this article, we highlight the need for behavioral health integration into care delivery and, more specifically, the patient-centered medical home. Details, inclusive of recommendations, are provided in an appendix on the interplay between behavioral health, chronic disease, substance abuse and palliative care.
Rationale for behavioral health integration
Among the multitude of reasons for behavioral health integration are:
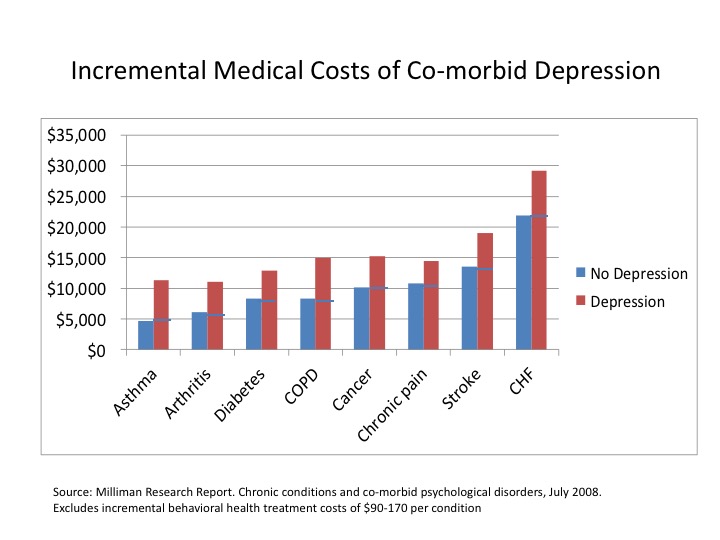
- Patients with co-morbid depression costs, on average, are 53 percent higher (range: 34 – 141 percent) than those with a chronic condition or cancer alone3
- The cost of major depressive disorders (MDD), estimated at $210 billion, is split between indirect costs (absenteeism, presenteeism) and direct treatment costs, including those associated with co-occurring anxiety, posttraumatic stress disorder (PTSD) and sleep disturbances4
- The high prevalence of mood disorders, anxiety and other clinical conditions5
- Mental Health America suggests “only 41% of individuals with any mental illness report receiving treatment and 20% felt they did not get the mental health services they felt they needed.”6
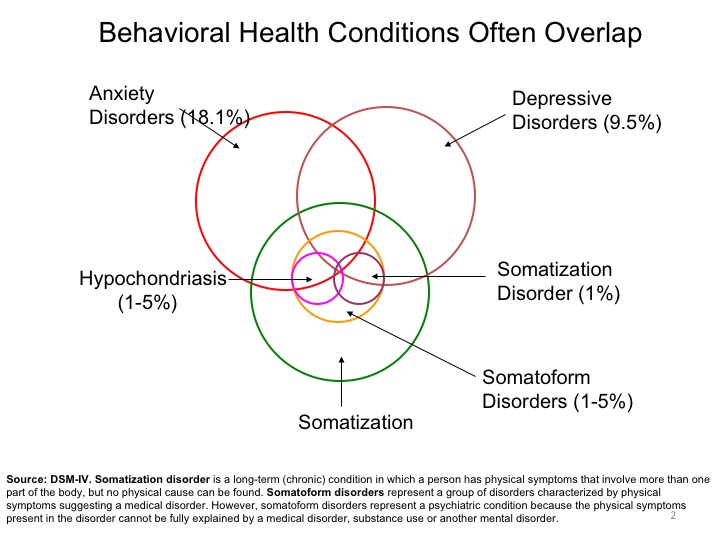
- The high cost of stress-related somatization disorders, affecting 1 – 5 percent of the population, presenting as physical symptoms7
- Increased patient activation, willingness to change and self-management; i.e., increased treatment compliance, lifestyle changes and earlier intervention
Behavioral health includes patient activation, engagement and self-management
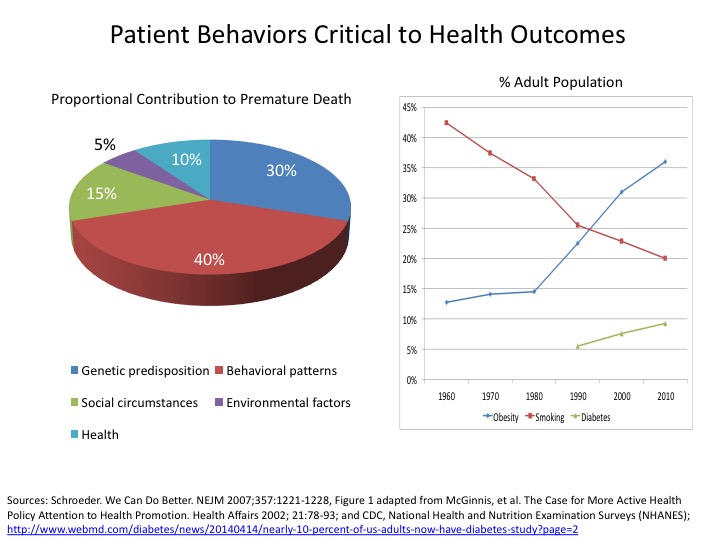
Patient behaviors, particularly lifestyle choices, are the leading contributor to premature mortality, morbidity and disability.8 The aggregate number of Americans with at-risk lifestyles is staggering: a poor diet and/or sedentary lifestyle contribute to obesity (72.0 million); cigarette consumption (45.3 million); illicit drug use, excluding marijuana (16.4 million); and "heavy" alcohol ingestion (15.0 million).9,10,11 Lifestyle change is difficult and requires health engagement at home, in the workplace and directly with providers.
The ability of a patient to become engaged in his or her healthcare depends not only on the quality and accessibility of providers, but also level of activation and willingness to change behavior.
In the current healthcare delivery system, primary care physicians have a limited amount of time to address the chronic care needs of patients, i.e., lifestyle issues, risk factors, co-morbidities and medications. The average face-to-face patient care time measured by direct observation was reported as 10.7 minutes, excluding visit specific work outside the examination room (2.6 minutes), figures far lower than the self-reported results of the National Ambulatory Medical Care Survey in 2003.12 Virtually no time is spent addressing nutrition, exercise, smoking cessation or mental health concerns.13,14 A more recent 2013 study suggests a downside of widespread electronic medical record (EMR) implementation is further erosion of “quality time” with patients.15
Patient activation, or having the knowledge, skills and confidence to manage one's health, is closely related to health outcomes.16 Knowledge alone is insufficient to facilitate significant behavioral change. Health literacy remains an issue, with nearly half of the adult U.S. population having difficulty understanding appointment slips, medical education brochures, physician directions, instructions on prescription drug bottles and consent forms.17 Psychosocial mediators such as self-efficacy, attitudes, health beliefs, mood, motivation and coping skills, and the degree of social support are also exceedingly important for patient activation and engagement.
According to the Prochaska and DiClemente Stages-of-Change Model, the practice of new behaviors (3 – 6 months) requires a commitment to maintenance (6 – 60 months) to avoid a relapse.18
Self-care is critical to the management of chronic diseases and conditions. According to the Agency of Healthcare Quality and Research (AHRQ), self-management requires making lifestyle changes; monitoring signs, symptoms and biometric measurements indicative of a potential change in health status; and taking action when warranted (e.g., taking medications, calling a caregiver or physician). A study evaluating depressed patients diagnosed within a primary care clinic highlighted a deterioration of the elements most necessary for self-management such as vitality, social functioning and emotional state.19
Mental health conditions are exceedingly common
According to the National Institute of Mental Health, mood disorders and anxiety affect 9.5 percent to 18.1 percent of the adult population in any given year.3 Mood may be elevated (mania, hypomania), depressed (major depressive disorders, dysthymia disorders) or cycled (bipolar, cyclothymia) in the same patient. Despite being highly treatable, 60 to 80 percent of people with major depression disorders are under-diagnosed or inadequately treated by physicians.20
Approximately 14.8 million adults (6.7 percent) live with major depression, 6.1 million (2.6 percent) have bipolar disorder and 42.0 million (18.1 percent) exhibit a range of anxiety disorders, such as panic disorder, obsessive-compulsive disorder (OCD), PTSD, generalized anxiety disorder and phobias.21 Somatization, a tendency to experience and communicate somatic (“body”) distress in response to psychosocial stress and to seek medical treatment, may accompany depression and anxiety. About 9.2 million (42.6 percent) of the 21.6 million adults with substance dependence and abuse disorders have co-occurring mental health disorders.22
Mood disorders may also occur in response to a medical condition. The risk of depression in patients with a serious medical condition is estimated at 25 – 33 percent.23 The rate varies by the type of condition (e.g., heart attack, stroke, cancer), its lifecycle and severity, presence of co-morbidities, impact on functional status, degree of psychosocial support and whether it is life-threatening or terminal. Non-medical risk factors also contribute to the underlying emotional state and include social isolation, bereavement, retirement, job loss, relocation and substance abuse, most commonly involving prescription medications and alcohol.
Patient fears associated with chronic and life-threatening illness include loss of control and self-image, the expression of anger, dependency, stigma, isolation, abandonment and death.24 If recognized, these symptoms can be treated with a brief, structured behavioral intervention based on principles of cognitive behavioral therapy. If unrecognized, patient fears may also contribute to the development of clinical depression and/or anxiety.
Depression in patients with chronic conditions poses diagnostic challenges. Symptoms such as weight loss, fatigue, loss of appetite, sleep alterations and pain may reflect the underlying condition and not be indicative of a behavioral health issue. Alternatively, unexplained symptoms such as shortness of breath, dizziness, chest or abdominal pain, headache, back pain and other somatic complaints may occur in more than half of patients with depression or anxiety.
More than 65 percent of antidepressants are prescribed by primary care physicians, and yet depression screening does not occur in most practices.25
Financial implications of behavioral health are significant
Disengaged and depressed patients are less likely to self-manage and adhere to care plans. The five factors of non-adherence include socio-economic, condition-related, therapy-related, patient-related and the healthcare system (team).26
Improved self-management of chronic diseases results in an approximate cost-to-savings ratio of 1:10.27
Patient nonadherence to prescribed medications often leads to suboptimal therapeutic outcomes and disease progression.28 The Center for Disease Control (CDC) estimates (a) 25 – 30 percent of prescriptions are never filled, (b) 50 percent of prescriptions are not continued as prescribed, (c) avoidable direct healthcare costs of non-adherence range between $100 billion – $289 billion and (d) costs per patient in physician visits due to non-adherence are $2,000 per annum.27
The Centers for Medicare & Medicaid Services (CMS) has launched initiatives focused on the total cost of care such as Accountable Care Organizations (7.7 million beneficiaries), Comprehensive Joint Replacement (90-day episode), Cardiac Care Episode Payment Model (bypass surgery, interventional procedures), Oncology Care Model (six-month episode, including drug costs), Million Hearts® Cardiovascular Disease Risk Reduction Model (population health) and the Home Health Value-based Purchasing pilot (five states, +/- 3 – 8 percent penalty or bonus). These initiatives are being implemented nationwide or mandated for targeted metropolitan statistical areas (MSA) and states. At-risk payment contracts are also increasingly being negotiated with commercial payers. The incremental costs of co-morbid behavioral health issues in patients with a chronic disease average 53 percent.3
The Million Hearts® Cardiovascular Disease Risk Reduction Model, targeting 3.3 million Medicare beneficiaries (20,000 practitioners), provides “targeted incentives for health care practitioners to engage in beneficiary CVD risk calculation and population-level risk management.” Predictive models will be used to randomize patients based on risk scores; 516 institutions from 47 states are participating.29
The financial implications of risk reduction in cardiovascular disease cannot be over-stated, as non-adherence to cardiovascular drugs causes 30 percent to 50 percent of treatment failures and 125,000 deaths annually. More specifically, non-adherence to statins causes an increased relative risk for mortality of 12 – 25 percent; non-adherence to cardio-protective medications increases the risk of cardiovascular hospitalizations (10 percent to 40 percent) and mortality (50 percent to 80 percent); and poor adherence to heart failure medications increases the number of cardiovascular-related emergency department (ED) visits.30
Recommendations
The essentials of patient engagement include the establishment of treatment goals based on shared decision-making, extending the social network to the caregiver, providing a web-based portal for provider access (appointments, test results, reminders, educational resources) and 24/7 communications. The availability of passive systems does not imply engagement. Strategies are especially important for high-risk and resource-intensive patients.
Patient drug adherence can be improved by simplifying the regimen, imparting knowledge, modifying patient beliefs and behavior, providing enhanced communication and trust, leaving the bias and evaluating adherence (SIMPLE).31
Barriers to effective behavioral health therapy include insufficient depression screening, inadequate primary care knowledge and an over-dependence upon prescription drugs, shortage of behavioral health providers and/or inadequate provider networks, limited awareness (knowledge) of mental illness by patients and their caregivers, the presence of stigma and financial requirements. Only 41 percent of patients with mental health issues receive treatment; 59 percent do not receive treatment. Primary care physicians treat 56 percent of patients, whereas mental health professionals treat the remaining 44 percent.32
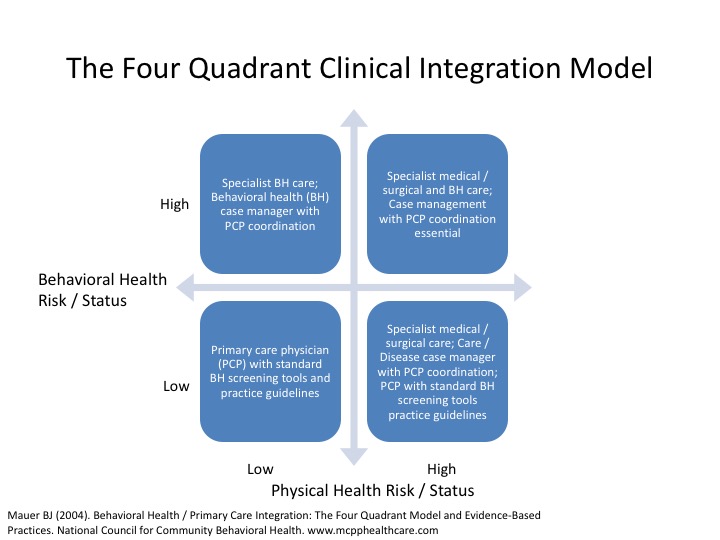
The four quadrant clinical integration model identifies provider requirements – physician (primary care, specialist) and care manager (behavioral health, medical / disease) – based on the behavioral health and physical health risk status.
The US Preventive Services Task Force (USPSTF), an independent panel of experts in primary care and prevention, recently updated its 2009 recommendation and “recommended screening for depression in the general adult population, including older adults and pregnant and postpartum women. Screening should be implemented with adequate systems in place to ensure accurate diagnosis, effective treatment, and appropriate follow-up.”33
Alternative medical and behavioral care delivery models include coordinated care, with referral behavioral services at a different location; co-located care, within a shared primary care location; and integrated care, with care teams comprised of behavioral health personnel, as necessary.33 Integrated care has been shown to be a cost-effective approach to addressing the needs of high-cost / risk patients.
Telehealth represents a viable option for the majority of patients with mild-to-moderate emotional and behavioral disorders, particularly in underserved rural and urban areas. Access remains a challenge given the growing shortage of adult and pediatric (adolescent) psychiatrists. Telemedicine has the potential to decrease the associated stigma, improve patient compliance with behavioral health referral, and increase the likelihood of sustained and non-pharmaceutical therapy. Collaborative care models ensure communications (and relationships) among primary care physicians, psychiatrists, other mental health providers and in more serious cases, the entire care team.
Appendix
Chronic Disease and Depression
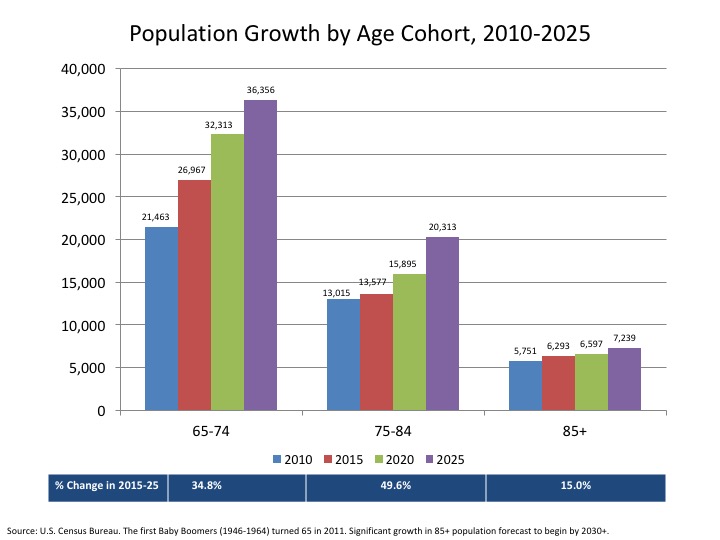
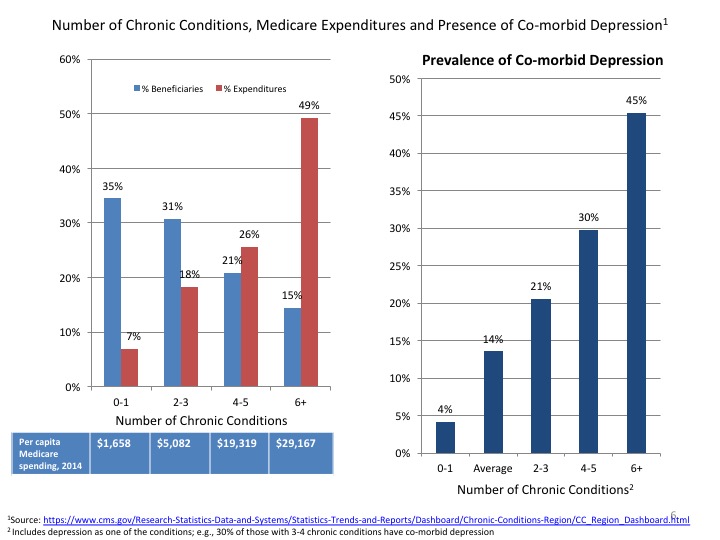
During the next decade, the population over the age of 65 is forecast to increase from 47.7 million in 2015 to 65.1 million in 2025 and represent 18.8 percent of the total.35 The rate of growth is highest for the 75 – 84-year-old cohort, followed by those 65 – 74 and over 85. Disease prevalence, as well as condition severity and complexity, increase with age. Medicare spending alone has been forecasted to increase from $646 billion in 2015 to $1,221 billion in 2024, reflecting a compound growth rate of 7.3 percent.36The vast majority of Medicare spending occurs in people with multiple chronic conditions.37
Among the chronic conditions affecting the Medicare population over 65 years old are hypertension (58.4 percent), hyperlipidemia (47.9 percent), arthritis (30.7 percent), ischemic heart disease (29.3 percent), diabetes (27.1 percent), chronic kidney disease (17.3 percent), depression (13.6 percent), Alzheimer’s disease and other dementias (11.5 percent) and chronic obstructive pulmonary disease (COPD) (11.0 percent).38 The prevalence of depression increases with the number of co-morbid conditions. For example, 30 percent of Medicare beneficiaries with three to four chronic conditions also have depression, as compared to less than 5 percent of those without other co-morbidities.
The prevalence of co-morbid depression also varies by acuteness of onset, type, severity and functional impact of a chronic condition.
Co-morbid depression has a significant impact on the total cost of care in patients for a multiplicity of reasons including a tendency to be less compliant with treatment plans, poorer lifestyles and the presence of medically undiagnosed physical symptoms (MUPS) (e.g., abdominal or chest pain, fatigue, dizziness, shortness of breath, headache). MUPS may vary in number, frequency, severity and location, and, as mentioned, pose diagnostic challenges to physicians. They often result in avoidable and inappropriate resource utilization.
Chronic Pain, Depression and Substance Abuse
Chronic (persistent) pain is exceedingly common and may be secondary to neuromuscular and/or joint injury (low back, neck, arthritis, neurogenic), imbalances in brain chemicals (migraines) and cancer.39 Approximately 7.5 million adults suffer from chronic low back pain for more than three months, of which 53 percent have functional limitations. 5.0 million adults have peripheral neuropathies secondary to diabetes or cancer, 2.5 million have moderate-to-severe neck pain, 7.9 million have symptomatic osteoarthritis (Grade 3 or 4 radiographic evidence) and 13.4 million report migraines, of which 4.0 million suffer from chronic daily headaches (at least 15 migraine days per month).40
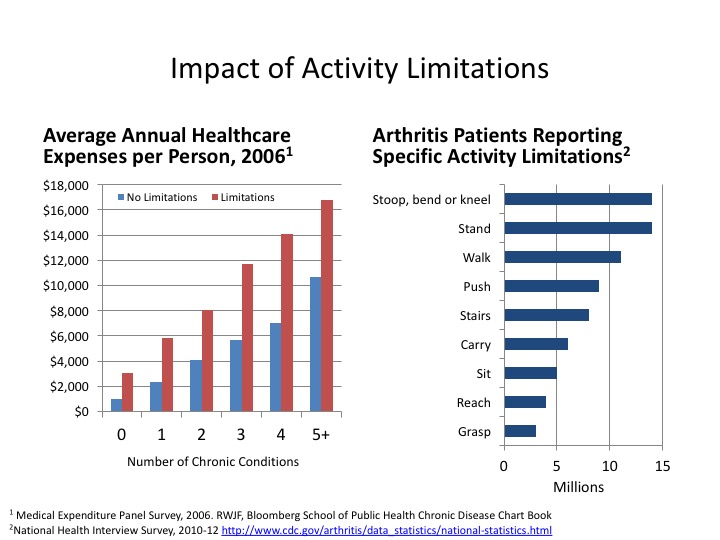
Pain often leads to limitations of usual activities, itself an independent driver of healthcare costs. For example, impairment due to arthritis may affect the ability of people to work, function in their community, or care for their family and contribute to behavioral health issues. According to Milliman Research, 21.9 percent of (sampled) patients with arthritis had depression – a figure consistent with more recent CDC study findings; i.e., 18 percent of patients had depression, whereas 31 percent exhibited anxiety.41 Medical spending, excluding the incremental cost of mental health therapy, was 82 percent higher in patients with arthritis and co-morbid depression as compared to patients with arthritis alone.42
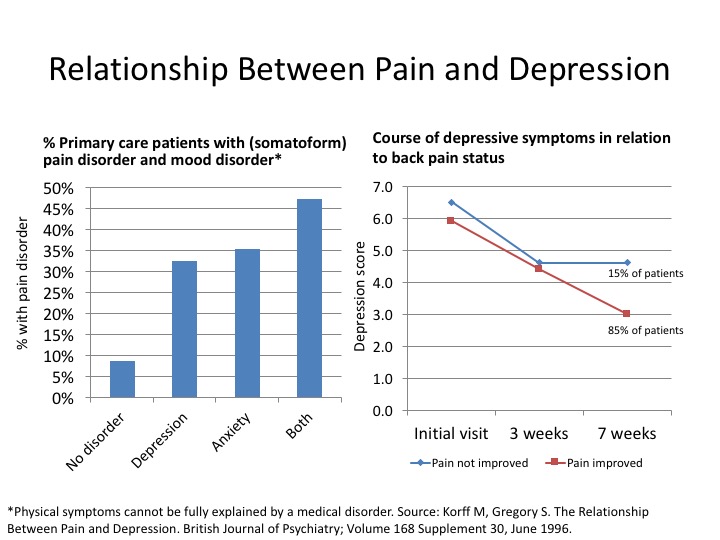
Pain and depression are related due to the involvement of specific neurotransmitters, serotonin and norepinephrine in the physiology of both conditions. Studies have shown that “people dealing with chronic pain run three times the risk of developing a mood disorder such as depression or anxiety.” About one-third of people with persistent pain experience clinical depression. Moreover, people with depression have three times the risk of chronic pain. When people have chronic depression over a long period of time, about one-half of them will develop chronic pain problems without any clear injury to explain that pain.43
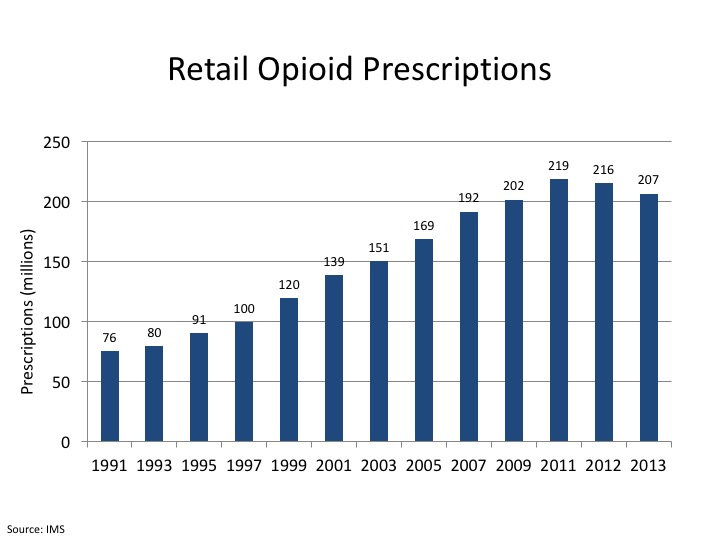
Historically, opioids were prescribed after surgery or for the treatment of terminal cancer pain. In the 1990s, drug companies and experts touting the safety of hydrocodone, oxycodone, oxycodone and acetaminophen, and meperidine for chronic pain and other indications (e.g., dental procedures) resulted in category revenue growth from $1 billion in 1992 to nearly $10 billion by 2015.44
The treatment of chronic pain with medications is not without risk due the possibility of drug tolerance, necessitating ever-higher doses; hyperalgesia or increased pain sensitivity; and substance abuse. The risk of addiction is unknown, with a reported range of 3 – 40 percent depending upon a variety of factors, e.g., population studied, duration of treatment, etc.45 Risk factors for addiction include a personal or family history of alcohol or drug abuse and age, i.e., being a teenager or young adult.
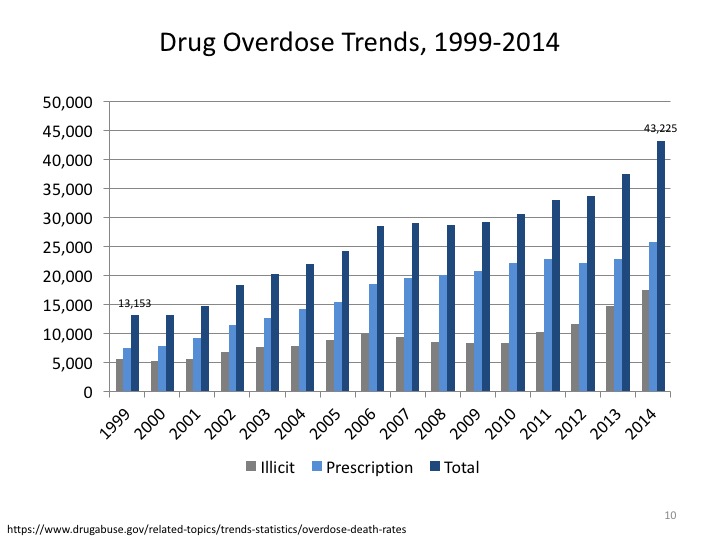
In 2009, approximately two million Americans exhibited dependence (tolerance and withdrawal) or addiction (compulsive drug use) to prescription opioids.46 ED visits have increased 2.8 times from 172,738 in 2004 to 488,000 in 2011; the number of admissions to substance abuse centers increased 3.3 times during the same period from approximately 55,000 in 2004 to 180,708 in 2011.47
In 2014, there were 43,225 deaths related to prescription (60 percent) and illicit (40 percent) drug overdose, more than triple the reported deaths (13, 153) in 1999.48 Opioids account for twice as many as heroin deaths, followed by benzodiazepines (e.g., Xanax, Valium) and cocaine.
Recommendations
- Significant diagnostic (e.g., MRI scans) and therapeutic (e.g., injections, surgical interventions and opioids) variation exists in the management of low back pain. Most patients will benefit from conservative treatment, i.e., physical activity and/or rehabilitation. It has been estimated that only 6 – 20 percent of acute back pain needs complex treatment (i.e., interventional radiology, orthopedic or neurosurgical), far below current practice. Evidence-based strategies to improve the quality, outcomes and cost-effectiveness have emerged, though implementation is lagging. Psychosocial factors have been shown to be a risk factor for developing chronic low back pain.
- Providers should use tools such as (a) The STarT Back Screening Tool (SBST), empirically proven to improve outcomes, which includes questions about the following: radiating leg pain, pain in the shoulder or neck, restricted walking, dressing more slowly than usual, fear avoidance, anxiety, pessimistic patient expectations, low mood and bothersomeness; and (b) the Oswestry Disability Index to track functional status. A return to normal activities as soon as possible is an indicator of a positive prognosis irrespective of pain levels.49
- Narcotic use increased from 19 percent of low back pain visits in 1999 – 2000 to 29 percent of visits in 2009 – 2010.43 Prescribing guidelines for opioids and chronic pain were released by the CDC in Match 2016.50 Chronic use of opioids may actually potentiate pain perception.
- Nearly one-half to two-thirds of substance use disorder (SUD) patients in treatment centers have a dual diagnosis inclusive of co-morbid mental health disorders such as depression, anxiety, bipolar disease, traumatic distress and/or conduct disorders (aggressive conduct and deceitful and destructive behaviors).51 Behavioral health treatment is essential to prevent relapse.
End-of-Life Care, Palliation and Depression
In 2012, there were 2.54 million deaths, with the number and rate increasing with age. Nearly three-quarters of deaths, 73.3 percent, were in people over 65 years old. Heart disease (23.6 percent) and cancer (22.9 percent) each account for approximately 0.6 million deaths per year or when combined, 46.5 percent of the total. Other leading causes of death include COPD (5.6 percent of the total), stroke (5.1 percent), accidents (5.0 percent), Alzheimer’s (3.3 percent), diabetes (2.9 percent) and influenza / pneumonia (2.2 percent).52 The majority of the Alzheimer’s and diabetes patients suffer from multiple co-morbidities, whereas influenza / pneumonia deaths often occur in debilitated, often bedridden patients.
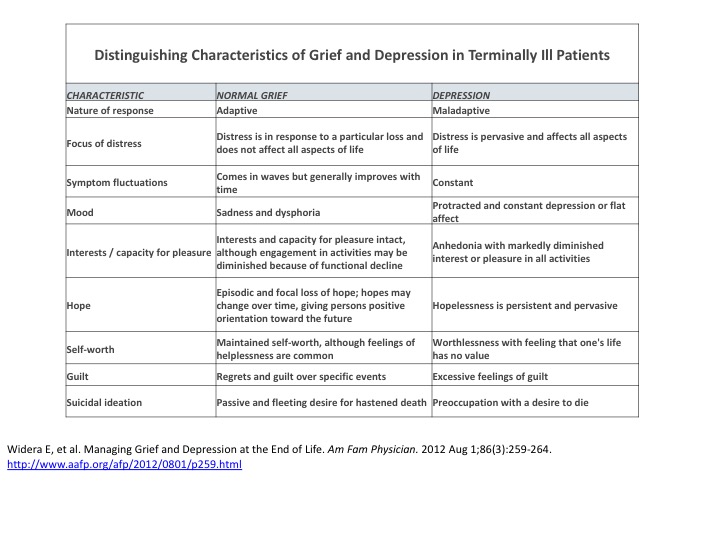
The prevalence of cancer and co-morbid major depression ranges from 5 to 30 percent; the pooled meta-analysis prevalence is 14 percent.53 The rate in congestive heart failure is 24 – 42 percent, whereas for COPD (e.g., emphysema, chronic bronchitis) it is 26 percent.54,55 Grief is a normal reaction to living with a terminal illness, whereas depression is not.
Discussion surrounding care at the end of life is an extremely personal experience for the patient, as well as his or her family and friends. Treatment objectives include “respecting patient preferences; providing comprehensive care; maximizing interdisciplinary resources; acknowledging caregiver concerns and creating a healthcare system flexible enough to support these goals.”56
According to a 2008 report to Congress, “there is substantial evidence that the treatment people would choose at the end of life commonly is different from the treatment they receive. Too often individuals receive more aggressive care than they desire.”57, 58 In fact, patients who discussed end-of-life care preferences had less fear and anxiety and were better able to influence and direct their own care.59
Aggressive care can negatively impact quality of life, affect caregivers and result in unnecessary hospitalizations, tests and procedures. In 2012, Medicare decedents represented 3.7 percent of beneficiaries, but accounted for a disproportionate 27.3 percent of total Medicare program expenditures (excluding decedent deductibles and co-payments) or $165 billion.60 The average Medicare program cost in the final year of life is $46,973 per person or 6.5 times the cost of surviving Medicare recipients.54 The figure rises to $53,295 with inclusion of patient deductibles and co-payments. The final three months of life account for 40.3 percent of total spending.61
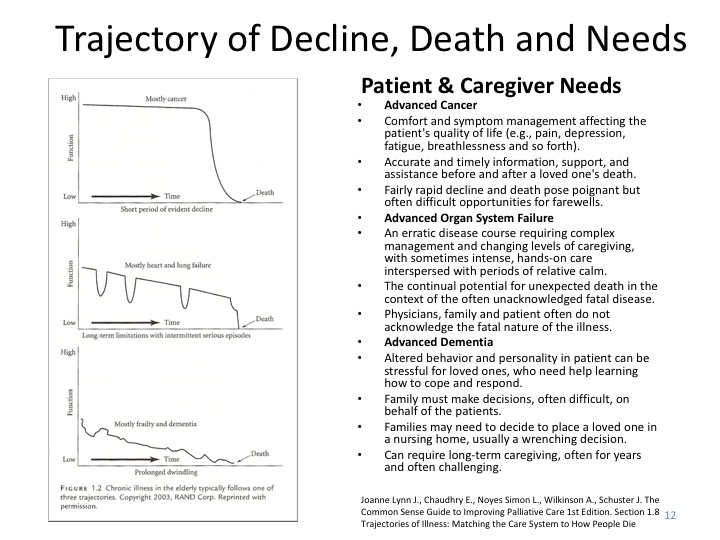
Opportunities exist to better organize healthcare service offerings with the presumed trajectory of death.62 The three major trajectories include cancer, organ failure (e.g., heart failure, COPD) and frailty with dementia. Cancer is most predictive.
According to the World Health Organization, “palliative care is an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.” It intends neither to hasten nor postpone death.63
Hospice care is a Medicare benefit. CMS criteria include voluntary participation, revocation and readmission; a presumed life expectancy of less than six months; and an agreement to forego conventional treatment for a terminal illness. The median length of hospice stay, 18.5 days, is far shorter than the mean (average) at 72.6 days; i.e., 34.5 percent have a length of stay of less than seven days, another 14.3 percent of between eight and 14 days and lastly, 12.7 percent between 15 and 29 days. Conversely, 11.5 percent exceed the six-month threshold.64 Hospice care is usually “too short” or “too long” relative to patient and caregiver needs.
Recommendation
- The majority of terminal patients are not depressed and remain capable of positive mood states.65 Psychotherapy, including cognitive behavior therapy and medications, should be used. Effective pain management remains essential.
References
1http://www.brainyquote.com/quotes/authors/w/william_osler.html
2Peek, CJ. National Integration Academy Council (2013). Lexicon for Behavioral Health and Primary Care Integration: Concepts and Definitions Developed by Expert Consensus. In Agency for Healthcare Research and Quality, AHRQ Publication No. 13-IP0001-EF
3Milliman Research Report. Chronic conditions and co-morbid psychological disorders, July 2008
4Barsky A, Orav EJ, Bates D. Somatization Increases Medical Utilization and Costs Independent of Psychiatric and Medical Comorbidity. JAMA Psychiatry; August 1, 2005 Vol 62 (8)
5National Institute of Mental Health. The Numbers Count: Mental Disorders in America. National Institute of Mental Health, May 2012. http://wwwapps.nimh.nih.gov/health/publications/the-numbers-count-mental-disorders-in-america.shtml#Intro
6Parity or Disparity: The State of Mental Health in America, 2015 http://www.mentalhealthamerica.net/sites/default/files/Parity%20or%20Disparity%202015%20Report.pdf
7Kuhl E. Quantifying the Cost of Depression. Partnership for Workplace Mental Health. http://www.workplacementalhealth.org/Publications-Surveys/Quantifying-the-Cost-of-Depression-.aspx
8Schroeder. We Can Do Better. NEJM 2007;357:1221-1228, Figure 1 adapted from McGinnis, et al. The Case for More Active Health Policy Attention to Health Promotion. Health Affairs 2002; 21:78-93
9http:www.cdc.gov/obesity/data/adult.html
10Centers for Disease Control and Prevention. 2011. Vital Signs: Current Cigarette Smoking Among Adults Aged ≥ 18 Years—United States, 2005–2010. Morbidity and Mortality Weekly Report; 60(35):1207–12
11SAMHSA. Nationwide Survey Shows Most Illicit Drug Users and Heavy Alcohol Users Are in the Workplace and May Pose Special Problems; 2007
12Gottschalk A, Flocke SA. Time spent in face-to-face patient care and work outside the examination room. Ann Fam Med. 2005;3(6):488–93.
13Yawn B, Goodwin MA, Zyzanski SJ, Stange KC. Time use during acute and chronic illness visits to a family physician. Fam Pract. 2003;20(4):474–7.
14Tai-Seale M, McGuire T. Time allocation in primary care with competing demands. Presented at the Economics of Population Health: Inaugural Conference of the American Society of Health Economists, TBA, Madison, WI, June 4, 2006.
15Healthcare IT News. Is your EHR damaging the patient-provider relationship? Physician concern points to a larger worry that EHRs can sometimes negatively affect the patient experience. November 14, 2014. http://www.healthcareitnews.com/blog/your-ehr-damaging-patient-provider-relationship
16Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012 May; 27(5):520-6
17National Network of Libraries of Medicine New England Region. Health literacy. http://nnlm.gov/outreach/consumer/hlthlit.html.
18UCLA Center for Human Nutrition. Prochaska and DiClemente’s Stages of Change Model. http/www.cellinteractive.com/ucla/physcian_ ed/stages_change.html.
19Patient Self-Management Support Programs: An Evaluation. Rand Health, November 2007. AHRQ Publication No. 08-0011 http://www.ahrq.gov/sites/default/files/publications/files/ptmgmt.pdf
20Kessler RC, et al. The Epidemiology of Major Depressive Disorder Results from the National Comorbidity Survey Replication (NCS-R). JAMA, 289(23): 3095-3105
21National Alliance on Mental Illness Fact Sheet http://www2.nami.org/factsheets/mentalillness_factsheet.pdf
22Substance Abuse and Mental Health Services Administration. (2012). Results from the 2010 National Survey on Drug Use and Health: Mental Health Findings NSDUH Series H-42, HHS Publication No. (SMA) 11-4667). Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2012.
23WebMD. Dealing with chronic illness and depression. http://www.webmd.com/depression/guide/chronic-illnesses-depression
24Polin I. Medical Crises Counseling: Short-term Therapy for Long-term Illness. New York: WW Norton, 1995
25R. C. Kessler, et all. Prevalence, Severity and Comorbidity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication (2005.) Archives of General Psychiatry, 62: 617-27
26World Health Organization. Evidence for Long-term Therapies, 2003 http://apps.who.int/iris/bitstream/10665/42682/1/9241545992.pdf
27Medication Adherence. CDC’s Noon Conference; March 27, 2013. https://www.cdc.gov/primarycare/materials/medication/docs/medication-adherence-01ccd.pdf
28Luga AO, McGuire MJ. Adherence and health care costs. Risk Manag Healthc Policy. 2014; 7: 35–44 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3934668/
29 CMS Million Hearts®: Cardiovascular Disease Risk Reduction Model. https://innovation.cms.gov/initiatives/Million-Hearts-CVDRRM/
30Ho 2009, Circulation; Edmondson 2013, Br J of Health Psychology; George & Shalansky 2006, Br J Clin Phar https://www.cdc.gov/primarycare/materials/medication/docs/medication-adherence-01ccd.pdf
31American College of Preventive Medicine. Medication Adherence Clinical Reference http://www.acpm.org/?MedAdherTT_ClinRef
32 Wang P et al. Arch Gen Psychiatry, 2005: 62. Adapted from Katon, Rundell, Unützer, Academy of PSM Integrated Behavioral Health 2014. Patient-centered Primary Care Collaborative Behavioral Health Task Force
33JAMA. Screening for Depression in Adults; US Preventive Services Task Force Recommendation Statement. January 26, 2016, Vol 315 (4) http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/depression-in-adults-screening
34Blount A (2003). Integrated primary care: Organizing the evidence. Families, systems and health: 21, 121-34.
35U.S. Census http://www.census.gov/population/projections/data/national/2014/summarytables.html
36CMS. CMS National Health Expenditures Page [internet]. Baltimore, MD: CMS; June 2016. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsProjected.html
37Robert Wood Johnson-Bloomberg School of Public Health Chart Book, February 2010. Chronic Conditions: Making the Case for Ongoing Care. Data sourced from Medicare Standard Analytic File (SAF), 2007
38Medicare Chronic Condition Dashboard, 2014 https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Dashboard/Chronic-Conditions-Region/CC_Region_Dashboard.html
39http://www.painmed.org/PatientCenter/Facts_on_Pain.aspx#common
40https://migraineresearchfoundation.org/about-migraine/migraine-facts/
41Centers for Disease Control and Prevention: Arthritis. National Statistics. http://www.cdc.gov/arthritis/data_statistics/national-statistics.html; and Morbidity and Mortality Weekly Report. Prevalence of Doctor-Diagnosed Arthritis and Arthritis-Attributable Activity Limitation — United States, 2010–2012 MMWR / November 8, 2013 / Vol. 62 / No. 44 http://www.cdc.gov/mmwr/PDF/wk/mm6244.pdf
42Alexandra Sifferlin. Arthritis Patients Often Have Anxiety and Depression Too. Time; May 1, 2012. http://healthland.time.com/2012/05/01/having-arthritis-often-means-suffering-from-depression-and-anxiety-too/
43Thompson D, Bass Pat MD MPH. The Link Between Pain and Depression. www.everydayhealth.com/pain-management/the-link-between-pain-and-depression.aspx
44http://www.nytimes.com/2016/05/21/health/opioid-prescriptions-drop-for-first-time-in-two-decades.html?_r=0.
45National Institute of Drug Abuse. Chronic Pain Treatment and Addiction. http://www.drugabuse.gov/publications/research-reports/prescription-drugs/chronic-pain-treatment-addiction
46http://www.health.harvard.edu/newsletter_article/painkillers-fuel-growth-in-drug-addiction
47https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates.
48http://www.rethinkopioids.com/prescription-opioid-abuse
49Foundation for Health Care Quality, Washington State Health Care Authority, November 2013 http://www.breecollaborative.org/wp-content/uploads/spine_lbp.pdf
50Thomas R. Frieden, M.D., M.P.H., and Debra Houry, M.D., M.P.H. Reducing the Risks of Relief — The CDC Opioid-Prescribing Guideline. N Engl J Med 2016; 374:1501-1504 http://www.nejm.org/doi/full/10.1056/NEJMp1515917?rss=mostViewed&#t=article
512013 National Survey of Substance Abuse Treatment Services and Chan,YF, Dennis ML and Funk RL. Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. Journal of Substance Abuse Treatment 34(1): 14-24, 2008
52National Vital Statistics Reports. Deaths: Final Data for 2012. Volume 63(9); August 31, 2015
file:///C:/Users/dgruber/Downloads/cdc_33063_DS1.pdf
53Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12(2):160–174.
54Guck TP, Elsasser G, Kavan M, Barone E. Depression and Congestive Heart Failure. CHF 2003; 9(3) http://www.medscape.com/viewarticle/456943
55Yohannes A, Alexopoulos G. Depression and anxiety in patients with COPD http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4523084/
56The Urban Institute. Medicare and End-of-life Care, 2002 http://www.urban.org/sites/default/files/alfresco/publication-pdfs/1000442-Medicare-and-End-of-Life-Care.PDF
57Advance Directives and Advanced Care Planning: Report to Congress, August 2008 https://aspe.hhs.gov/basic-report/advance-directives-and-advance-care-planning-report-congress
58U.S. Department of Health & Human Services, Office of Disability, Aging & Long-term Policy (DALTCP), Office of the Assistant Secretary for Planning and Evaluation (ASPE)
59AHRQ, Research in Action, Issue 12. Advance Care Planning.
http://www.ahrq.gov/research/endliferia/endria.htm
60Spending in the Last Year of Life and the Impact of Hospice on Medicare Outlays: Analysis of a decade of Medicare data ending 2013, and assessment of the impact of hospice on Medicare costs. June 22, 2015. Table 1-1
http://medpac.gov/documents/contractor-reports/spending-in-the-last-year-of-life-and-the-impact-of-hospice-on-medicare-outlays-rev.pdf
61Calfo S, Smith J, Zezza M. CMS Office of the Actuary. Last Year of Life Study, 2001. https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/downloads/Last_Year_of_Life.pdf
62Joanne Lynn J., Chaudhry E., Noyes Simon L., Wilkinson A., Schuster J. The Common Sense Guide to Improving Palliative Care 1st Edition. Section 1.8 Trajectories of Illness: Matching the Care System to How People Die http://www.mywhatever.com/cifwriter/library/commonsense/commonsense108.html
63 http://www.who.int/cancer/palliative/definition/en/
64MEDPAC Report to Congress, 2014 http://medpac.gov/documents/reports/mar14_entirereport.pdf?sfvrsn=0
65 Widera E, et al. Managing Grief and Depression at the End of Life. Am Fam Physician 2012 Aug 1;86(3):259-264.http://www.aafp.org/afp/2012/0801/p259.html