Implications of the IMPACT Act of 2014
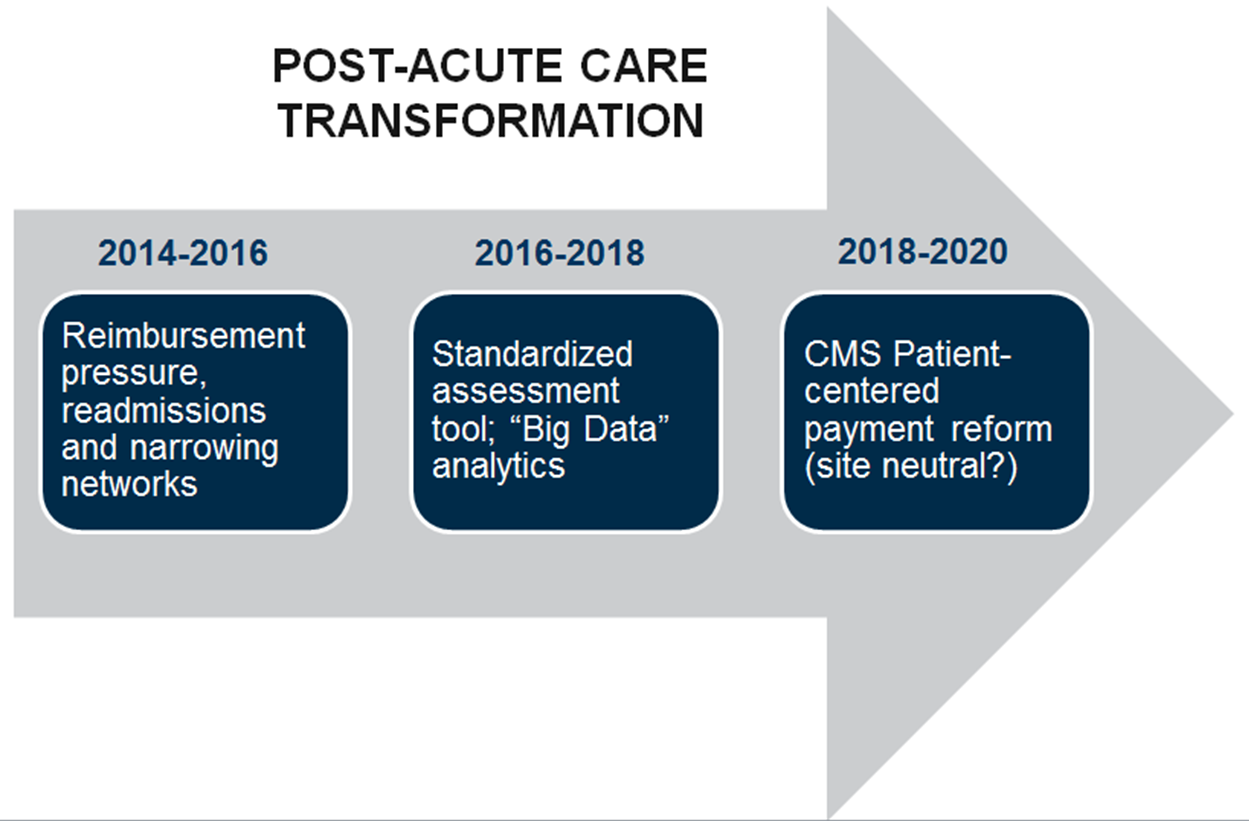
Post-acute care service providers — skilled nursing facilities, home health, inpatient rehabilitation facilities and long-term acute care hospitals — are currently in flux, given the Centers for Medicare and Medicaid Services (CMS) reimbursement cuts, the growth of Medicare Advantage, payment reforms such as Accountable Care Organizations and re-admission penalties, hospital consolidation and narrowing provider networks.
These issues are a precursor to the fundamental changes proscribed for the 2016-2020 period catalyzed by recent passage of the Improving Medicare Post-Acute Care Transformation Act (or the IMPACT Act of 2014), including the creation of a standardized assessment tool across all post-acute settings, the use of “big data” to increase cost-effectiveness, consideration of socio-economic (psychosocial) factors and the likely implementation of patient-centered payment schema. Strategic transformation is inevitable.
Background
In July 2013, the Institute of Medicine (IOM) published a seminal report entitled “Variation in Healthcare Spending: Target Decision Making, Not Geography” and found that higher spending in Medicare primarily comes from the “variation in utilization of post-acute care services and, to a lesser extent, by variation in the utilization of acute care services.”1 The report was generated following more than 20 years of evidence generated by the Dartmouth Atlas of Healthcare, highlighting significant variation in Medicare FFS spending (by state, metropolitan statistical area, hospital referral region, hospital and type of service) without an apparent relationship to clinical outcomes.2
The IOM Committee calculated a Medicare fee-for-service spending variation of 42 percent, a figure consistent with Medicare Advantage data that suggests a variation of a 36 to 50 percent. Post-acute care service providers account for 73 percent of the total variation in spending. The impact of reducing the differential utilization of other healthcare services among Medicare FFS recipients, such as diagnostic tests, procedures and prescription drugs, was minor.
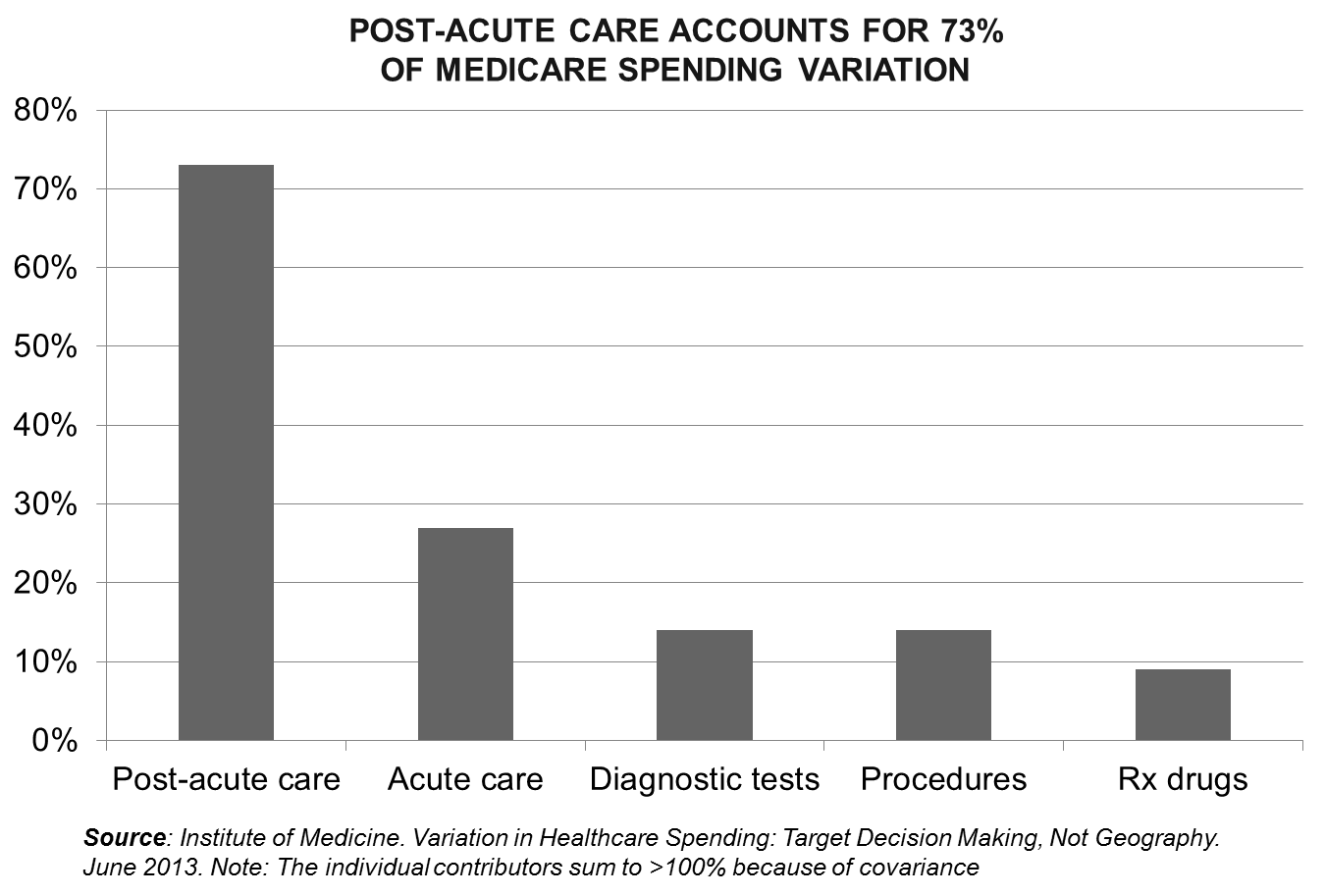
The IOM Committee recommended continued testing of payment reforms that “incentivize the clinical and financial integration of healthcare delivery systems” and encourage (a) care coordination among providers (b) real-time sharing of data, and tracking of service use and health outcomes (c) distribution of provider payments and (d) risk sharing/management across the care continuum.
Key Takeaways from the IMPACT Act
Congressional approval of H.R. 4994, the IMPACT Act ,mandates the development and implementation of a standardized post-acute care assessment tool, and requires the Medicare Payment Advisory Commission (MedPAC) to (1) evaluate and recommend to Congress features of post-acute care (PAC) payment systems that establish, or a unified PAC payment system that establishes, payment rates according to characteristics of individuals instead of according to the PAC setting, where the Medicare beneficiary involved is treated; and (2) recommend to Congress a technical prototype for a PAC prospective payment system.
According to the IMPACT Act, PAC providers include home health agencies (12,200), skilled nursing facilities (15,700), inpatient rehabilitation facilities (1,166) and long-term acute care hospitals (412). The majority of these providers are for-profit. The legislation excludes assisted living and similar residential care communities (22,200) and adult day service centers (4,800). The supply of nursing home and residential care beds varies by region.3
A standard acute care instrument, effective October 2016, would incorporate elements from the MDS (skilled nursing facilities), OASIS (home health agencies) and IRF-PAI (consisting of items from the Functional Independence Measure for inpatient rehabilitation facilities). Each of these tools utilizes “different terminology and definitions in describing functional ability, as well as different scales for quantifying disability.” They also measure different health domains, and items within similar domains are assessed differently (e.g., time period). 4
A uniform PAC assessment instrument would (1) clarify goals of care, incorporate patient (caregiver) preferences and enhance discharge planning; i.e., placement decisions, (2) facilitate transition management through interoperable core data transfer and (3) allow for the generation of longitudinal data analytics (e.g., outcomes, cost-effectiveness of alternative settings).
A Holistic and Comprehensive Approach
Standardized quality measures of CMS interest include (but are not limited to) functional status, cognitive status, skin integrity, medication reconciliation, major falls, “accurately communicating the existence of and providing for the transfer of health information and [patient, caregiver] care preferences” — the latter potentially inclusive of site of care and treatment alternatives such as palliative care.5
The standardized patient assessment instrument also includes (a) special services, treatments and interventions including the need for ventilator use, dialysis, chemotherapy, central line placement and total parenteral nutrition, (b) medical conditions and co-morbidities, and (c) impairments such as the ability to hear, see and swallow.
The assessment, at least as currently described, does not adequately consider the Medicare beneficiaries socio-economic psychosocial status, living situation and lifestyle — additional determinants of health outcomes and treatment (facility) optimization.
This assessment reporting will incorporate resource use measures, such as risk-adjusted spending per Medicare beneficiary and preventable hospital re-admission rates. A formal CMS analysis of the relationship between Medicare claims and patient assessment data will be completed by late-2018.
Patient-Centric Payment Reform
Using data from a variety of sources, the Medicare Payment Advisory Commission is required to submit to Congress (by June 30, 2016) a technical prototype PAC payment system. The system will be required to “establish payment rates according to the characteristics of individuals (such as cognitive ability, functional status and impairments), instead of the post-acute care setting where the Medicare beneficiary involved is treated.”5 Revisions to the payment proposal will be generated by CMS (with input from MedPAC) no later than two years after the collection of standardized patient assessment data (estimated: October 2018). A new payment system is likely by 2020.
Conclusion
PAC providers are being challenged by near- and longer-term issues. In the near-term, reimbursement pressures and penalties, and the emergence of narrow networks mandate efforts to increase the efficiency and effectiveness of care delivery.
In the longer term, a fundamental transformation of the PAC industry is imminent. “Big data” is upon us. A standardized patient assessment instrument across settings in 2016 will facilitate the determination of site cost-effectiveness. The Federal government, as the major payer of post-acute care services, is uniquely positioned to create a value-oriented, patient-centric PAC delivery system. Patient needs, combined with the ability of an agency or facility to best meet those needs on a cost-effective basis, will emerge as the driver of market success.
___________________________________________________________________________________
1 Variation in Healthcare Spending: Target Decision Making, Not Geography (slide presentation); Institute of Medicine of the National Academies
2Understanding of the Efficiency and Effectiveness of the Health Care System; The Dartmouth Atlas of Healthcare
3 National Center for Health Statistics. Long-term Care Services in the U.S.: 2013 Overview
4 Division of Health Care Policy and Research, University of Colorado at Denver and Health Sciences Center. Final Report: Uniform Patient Assessment for Post-Acute care; Jan. 25, 2006
5 H.R. 4994. 113th Congress of the U.S. “An Act to amend Title XVIII of the Social Security Act to provide for standardized post-acute care assessment data for quality, payment and discharge planning and for other purpose.” Jan. 3, 2014